Understanding the Basics of Medicare Redetermination
Medicare redetermination is an important process that reassesses an individual’s eligibility for the Medicare program. This serves to ensure that beneficiaries still meet the necessary qualifications for receiving benefits. When changes occur in an individual’s circumstances, such as income or household size, it may trigger a redetermination. During this process, applicants may need to provide updated information and documentation. Understanding this procedure is crucial for beneficiaries to maintain their coverage and avoid any disruptions in their healthcare services. Beneficiaries should be aware of the importance of timely and accurate submission of all required documents. Engaging in this process proactively can prevent potential lapses in coverage. Being informed about redetermination helps beneficiaries stay prepared, ensuring continuous access to essential medical services without unnecessary interruptions.
Eligibility Criteria for Medicare Redetermination
Medicare redetermination often involves revisiting the eligibility criteria based on current standards. Eligibility typically requires individuals to be of a certain age, usually 65 or older, or to qualify due to a disability or specific health conditions. Income levels and other personal circumstances, such as residency status and legal documentation, also play a critical role in determining eligibility. Ensuring that these criteria are met is essential for the approval of continued benefits during a redetermination process. Changes in these criteria can affect eligibility, and beneficiaries need to be aware of such updates. Proactive understanding of eligibility requirements supports a smoother redetermination process. Individuals should regularly review their eligibility status to accommodate any life changes, ensuring that they remain qualified under the current Medicare rules and regulations.
Step-by-Step Guide to the Redetermination Process
The Medicare redetermination process can be broken down into several key steps that beneficiaries should follow closely. Initially, it begins with receiving a notice from Medicare requesting updated information. The next step involves gathering all relevant documents to demonstrate continued eligibility, such as proof of income, identification, and residency status. Carefully completing and submitting the required forms by the specified deadline is also crucial. After submission, a review period follows where Medicare evaluates the provided information. It is important for beneficiaries to be diligent and responsive, addressing any additional requests from the Medicare office promptly. Following these steps ensures a comprehensive response to Medicare’s requirements, aiding in a successful redetermination. Meticulous attention to detail during this process can prevent complications, such as denial of benefits or coverage interruptions.
Common Challenges and How to Overcome Them
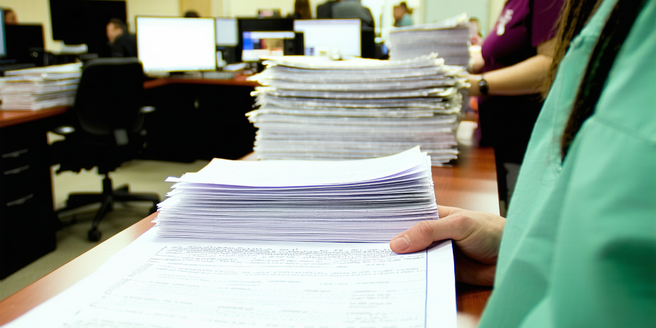
Medicare redetermination can present several common challenges, but being prepared can help overcome them effectively. One frequent issue is the complexity and volume of required paperwork, which can be daunting for many beneficiaries. To tackle this, organizing documents well in advance and seeking help from support services can be highly beneficial. Misunderstandings about eligibility criteria or changes in them can also pose challenges. Staying informed through credible sources and consulting with Medicare specialists can alleviate these concerns. Another potential hurdle is the tight timelines for submitting information. Beneficiaries should set reminders to ensure they meet all deadlines. Proactively addressing these challenges by being organized, informed, and timely can prevent potential disruptions in coverage and ensure a smoother redetermination experience.
Timelines and Deadlines You Need to Know
Adherence to timelines and deadlines is critical in the Medicare redetermination process. Once a redetermination notice is received, beneficiaries are typically given a specific period to submit all necessary documentation. This period can vary but usually spans several weeks. Failing to complete the redetermination within this timeframe can result in delayed or denied benefits. It is essential to pay close attention to the dates specified in the notice and plan document submission accordingly. Keeping a calendar reminder is advisable, ensuring all information is collected, reviewed, and submitted well ahead of the due date. Timely submission not only aids in maintaining uninterrupted benefits but also provides peace of mind, ensuring beneficiaries remain covered and continue to receive essential healthcare services without unnecessary stress.
Resources and Support for Medicare Beneficiaries
Navigating the Medicare redetermination process can be challenging, but numerous resources and supports are available to assist beneficiaries. Government helplines and local Medicare offices offer direct guidance and can answer specific queries related to form submissions and eligibility. For more complex issues, seeking advice from health insurance counselors or legal advisors specializing in Medicare can be beneficial. Community organizations and advocacy groups dedicated to healthcare rights also provide valuable resources. These groups often offer workshops, informational sessions, and one-on-one support to help beneficiaries understand the process more thoroughly. Utilizing these resources can demystify the redetermination process and ease the burden on beneficiaries, ensuring they have the support needed to maintain their Medicare benefits without undue difficulty.
